Procedures
The following procedures are available at Mead Medical:
- Ear Microsuction
For removal of excess wax in the ear canal. - Ferinject Infusions
This is an Iron replacement given by IV to people who are low in Iron. - Insertion & Removal of Implanon Contraception Device
Is a hormonal Implant that can provide long term birth control. It is a soft plastic stick about 4cm long, inserted into the upper arm & slowly releases a type of hormone – progestogen - Insertion & Removal of IUD Contraception, including Mirena
Is a hormonal Intrauterine device (IUD) that can provide long term birth control. It is a “T” shaped plastic frame that’s inserted into the uterus, where it releases a type of hormone progestin - Minor Wound Repairs
Including suturing superficial lacerations - Removal of Skin Lesions
Including Sebaceous Cysts, Lipomas and/or potential Skin Cancers - Tongue Tie Release & Lip Tie Release
Is a condition in which the thin piece of skin under the tongue/lip is abnormally tight. The operation involves releasing the skin under the Tongue/Lip. - Venesections
Is an act of drawing blood for treatment of Blood Disorders. - Vasectomy
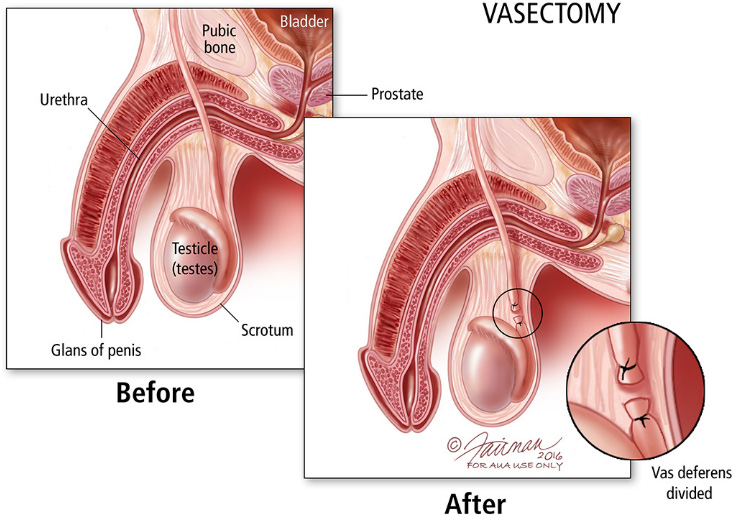
Is an operation that prevents sperm travelling from the testicles to the penis. It is done by cutting the tubes that allow sperm to leave the testicles. This process is also known as male sterilisation, or ‘the snip’.
Fees for these services vary depending on the provider of the service. For full information on fees please enquire with staff.
Patient Information – Vasectomy
What is a Vasectomy?
A vasectomy is an operation that prevents sperm travelling from the testicles to the penis. It is done by cutting the tubes that allow sperm to leave the testicles. This process is also known as male sterilisation, or ‘the snip’. Vasectomy is more than 99 per cent effective at preventing pregnancy.
Treatment
Vasectomies can be done at Mead Medicals procedural rooms. You will be asked to sign a form that gives your GP permission to do the procedure.
In the procedure room, you shave the scrotal area. Local anaesthesia will be injected to numb the area, but you’ll be aware of touch, tension, and movement. The local anaesthetic should block any sharp pain. If you feel pain during the procedure, you can let your GP know so you can get more anaesthesia.
What are the Risks?
Right after surgery, there’s a small risk of bleeding into the scrotum. If you notice that your scrotum has gotten much bigger or you are in pain, call your GP right away. If you have a fever, or your scrotum is red or sore, you should have your GP check for infection. There is a small risk for post-vasectomy pain syndrome. This occurs in 1 or 2 men out of 100 vasectomies. Post-vasectomy pain syndrome is a pain that can follow a vasectomy. It isn’t clear what causes this in many cases, but it’s most often treated with anti-swelling meds. If this occurs, see your GP as sometimes the specific cause can be treated with medicine or a minor procedure.
Studies show men who have had a vasectomy are not at a higher risk for any other medical conditions such as heart disease, prostate cancer, testicular cancer, or other health problems.
What to expect After Treatment
After your vasectomy, you may be uncomfortable for a few days. To reduce your pain, you may need mild pain medication to take care of any pain. Severe pain may suggest infection or other problems and you should see your GP. You may have mild pain like what you’d feel like several minutes after getting hit “down there.” A benign lump (granuloma) may form from sperm leaking from the cut end of the vas into the scrotal tissues. It may be painful or sensitive to touch or pressure, but it isn’t harmful. Most of the time, you don’t feel pain and this usually gets better with time.
Your GP will give you instructions for care after a vasectomy. Most men go home right away after the procedure. You should avoid sex for 1 week or activities that take a lot of strength. Swelling and pain can be treated with an ice pack on the scrotum and wearing a supportive undergarment, such as a jockstrap. Most men fully heal in less than a week.
Sex can often be resumed within a week after the vasectomy, but it’s important to know that a vasectomy doesn’t work right away. After the vasectomy, new sperm won’t be able to get into the semen, but there will still be lots of sperm “in the pipeline” that takes time to clear. You should follow up with your GP for semen analysis at 3 months to check for sperm in your ejaculate. During this time, you should use other forms of birth control.
The time it takes for your ejaculate to be free of sperm can differ. Most GPs suggest waiting to check the semen for at least 3 months. One in 100 men will still have sperm in their ejaculate at that time and may need to wait longer for the sperm to clear. You shouldn’t assume that your vasectomy is effective until a semen analysis proves it is.
- No sex or ejaculation for 7 days after the operation
- No swimming or baths in the first week
- Have quick showers in and out and keep the dressing intact for 3-4 days You may get a small drop or two of blood in the ejaculate during the first 1-2 months post-op, this is normal and of no concern unless it continues beyond 2 months or is very heavy (ejaculate becomes red)
- You can have 1-2 alcoholic drinks per day but do not exceed this in the first 7 days
When can I return to work and resume activities?
Some men may return to work a day or two after a vasectomy, especially if the work mainly involves sitting at a des. If your work involves any kind of lifting, reaching, stretching, or other physical exertion you will need to request light duties for your first week of return. If this is not possible, you will need to take the week off work. Remember to ask for a medical certificate during your consultation, if required.
You should avoid any physically strenuous activities for a week after your procedure, including walking and standing all day, or carrying more than 10-15kg.
Avoid non-contact sport (golf, tennis, running, swimming) or carrying more than 20-30kg for 2 weeks after your procedure. Avoid road cycling for the firs 3 weeks, although cycling on a stationary trainer bike is permissible after 2 weeks.
You cannot resume contact sport (rugby, soccer, football, martial arts) mountain biking or heavy weightlifting until 1 month after your procedure.
FAQs
Can my partner tell if I have had a vasectomy?
Sperm adds very little to the semen volume, so you shouldn’t notice any change in your ejaculate after vasectomy. Your partner may sometimes be able to feel the vasectomy site. This is particularly true if you have developed a granuloma.
Will my sense of orgasm be changed by having a vasectomy?
Ejaculation and orgasm are not affected by vasectomy. The special case is the rare man who has developed post-vasectomy pain syndrome.
Can I develop erectile dysfunction after a vasectomy?
A vasectomy does not cause erectile dysfunction.
Can a vasectomy fail?
There is a small chance a vasectomy may fail. This occurs when sperm leaking from one end of the cut vas deferens find a channel to the other cut end. Once your GP clears you with a sperm test showing no sperm or less than 100,000 sperm, with none moving, the risk of pregnancy is 1 in 2000.
Can something happen to my testicles?
In rare cases, the testicular artery may be hurt during vasectomy. Other problems, such as a mass of blood (hematoma) or infection, may also affect the testicles.
Can I have children after my vasectomy?
Yes, but if you haven’t stored frozen sperm you’ll need an additional procedure. The vas deferens can be surgically reconnected in a procedure called vasectomy reversal. This procedure would not be covered by Medicare except under special circumstances. If you don’t want to have vasectomy reversal, sperm can be taken from the testicle or the epididymis and used for in vitro fertilization. These procedures are costly and may not be covered by your health plan. Also, they don’t always work. If you think you may want to have children one day, you should look into non-permanent forms of birth control before deciding to have a vasectomy.